Mali, Africa: Dog Meat And Now Ebola
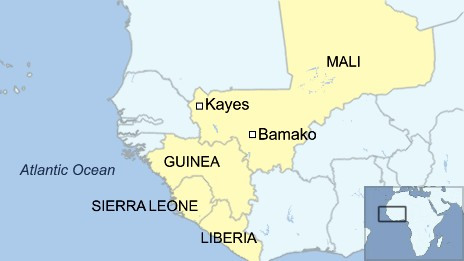
Ebola has now arrived in the country of Mali, West Africa, sparking further panic as the deadly virus creeps across the continent. The patient is a 2-year-old girl who was brought from neighbouring Guinea after her mother died of Ebola.
The girl showed symptoms, including a bleeding nose, while travelling on a public bus through several towns, as she travelled more than 1,000 km (600 miles) from Guinea through the capital, Bamako, to Kayes.
Bamako is a densely-packed city of 2.3 million people.
The girl’s blood sample tested positive in Fousseyni Daou hospital in the western town of Kayes,, where a further 43 people are being quarantined, including 10 health workers. Mali is now the sixth West African country to be fighting Ebola. The World Health Organisation says the disease has infected nearly 10,000 people and killed from half to 70 percent of them.
Dog Meat and Ebola
Dog meat is eaten in Mali and served at many “chop shops.” There is a link between Ebola and dog meat.
Dogs do not show any signs if infected with Ebola and dogs do NOT die from Ebola infections.

African dog butcher brutally slaughtering a dog for dog meat; the dog was in agony and fully conscious for several minutes.
Saynotodogmeat.Net Director Dr. Josa Depre advises that people refrain from eating dogs within Ebola infected zones. “Consuming dogs within an infected zone and knowing both dog can carry and show no signs is no different to playing Russian Roulette with one’s life,” says Dr. Depre.
Dogs in Africa are typically kept as pets to assist with hunting and are not “fed,” and therefore forced to scavenge food for themselves. In places like Liberia for example, dogs eat the carcass of Ebola infected animals and those same dogs are then captured by dog snatchers and sold for human consumption.

African dog butcher slowly slaughtering a dog, using a panga. Fully conscious, the dog was alive and in great agony for several minutes.
To date there have been no documented infections in felines, meaning that our domestic cats are probably safe from it.
Although dogs are susceptible to Ebola, the CDC concluded that “infected dogs are asymptomatic”, meaning that they do not develop symptoms.
During the early phase of their infection, however, they can spread the disease to humans and other animals through licking, biting, urine, and feces. However, the good news is that once the virus is cleared from the dog it is no longer contagious.”
Chop Shops In Mali
In San, Mali, there’s a restaurant in the old Bamabus terminal at the intersection turning south from the center of town. San is part of the Bobo ethnic area where dog meat is regularly served and eaten “as beef.” Restaurant reviews in Mali suggest that if you do not want to eat dog meat then you should stay away from ALL beef dishes, especially “chop shops” in certain areas, as a lot of the so-called beef is dog meat.
Guinea, which hasn’t closed any of its frontiers with six other nations, shares more than 800km of border with landlocked Mali to the east.
Ebola
Vaccines are not available until the first half of 2015, which is cold comfort for those who need vaccines immediately. Media statements such as “committed to ramping up production” by pharmaceutical companies are hollow words until the vaccines are actually produced and in use.
In America a New York doctor, Dr Craig Spencer who returned from Guinea on October 17th, has tested positive for Ebola, sparking terror amongst Americans after it was announced that the doctor had been travelling on the subway, possibly infecting other people. He is the first Ebola case diagnosed in New York, and the fourth in the US. On Tuesday he began to feel tired and developed a fever and diarrhoea on Thursday (BBC.)
The Ebola fatality rate can reach 90% - but current outbreak has mortality rate of about 70%. Incubation period is two to 21 days and there is no proven vaccine or cure. The current outbreak is the deadliest since Ebola was discovered in 1976.
An international team of scientists has been set up to determine the effectiveness of using the blood of Ebola survivors as a treatment. It is hoped the antibodies used by the immune system to fight Ebola can be transferred from a survivor to a patient.
How Not To Catch Ebola:
* Avoid direct contact with sick patients as the virus is spread through contaminated body fluids
* Wear protective cover for eyes
* Clothing and clinical waste should be incinerated and any medical equipment that needs to be kept should be decontaminated.
* People who recover from Ebola should abstain from sex or use condoms for three months
As with all the other Ebola infected areas, people in Mali are being urged to use soap when washing their hands. It is not customary to do this in Mali, but the World Health Organisation are stressing the importance of it.
All the African countries affected by Ebola are dog eating countries. There is a link between Ebola and dog meat.
DO NOT EAT DOG MEAT!
Thank you for reading,
Michele Brown.
GLOBAL MARCH
Saturday April 4th, 2015 Saynotodogmeat.Net is hosting a Global March for dogs and cats in the live meat trade. Please march with us, in your country. It will be an orderly and peaceful march but we need more ‘demonstration leaders.’ If you can help us, PLEASE EMAIL: CONTACT@SAYNOTODOGMEAT.INFO
Bring your family, children, pets and banners; we need as many people as possible, worldwide. Please mark your calendar and join our march. If you haven’t already done so, please click the box to let us know you are coming: https://www.facebook.com/events/294347744053559/
SAYNOTODOGMEAT.NEt NOW ACCEPTING DONATIONS
Saynotodogmeat.Net is now accepting donations: PLEASE MARK ALL DONATIONS “SAY NO TO DOG MEAT.NET” https://www.facebook.com/SayNoToDogMeat/app_117708921611213
No donation is too small and we are very appreciative of your help and support. Very soon we will be writing a full article outlining where donations will be used. You will receive an electronic receipt and we will too, which we will keep for historical data purposes. NO DONATION will be used to produce clothing with logos on, badges or banners. Donations are NOT for the directors. ALL MEMBERS FUND THEMSELVES.
PLEASE CONTINUE TO SIGN AND SHARE SAYNOTODOGMEAT.NET PETITIONS; WHEN COMPLETED THEY WILL BE HAND DELIVERED
PETITION FOR SOUTH KOREA
https://www.change.org/en-GB/petitions/president-geun-hye-park-take-dog-cat-meat-off-the-menu
PETITION FOR VIETNAM and THAILAND ANTI-SMUGGLING
https://www.causes.com/actions/1764795-a-petition-to-president-truong-tang-sang-moj-prime-minister-yingluck-shinawatra
PETITION FOR HEALTH MINISTER OF VIETNAM
https://www.causes.com/campaigns/71258-minister-of-public-health-thi-kim-tien
PETITION FOR NAGALAND
https://www.change.org/en-GB/petitions/additional-chief-secretary-take-dog-meat-of-nagaland-menu
PETITION TO BAN THE TRADE IN NIGERIA
https://www.change.org/en-GB/petitions/governor-of-lagos-hon-babatunde-fashola-ban-the-nigerian-dog-meat-trade-lagos
LETTER TO THE PRESIDENT OF THE PHILIPPINES
http://saynotodogmeat.net/2014/04/04/email-the-philippines-president-to-end-the-dog-meat-trade/
PLEASE SEND TO THE MUSLIM COUNCIL
http://saynotodogmeat.net/2014/01/17/open-email-to-the-muslim-council-of-great-britain/
PLEASE HELP THE PEOPLE OF TURKANA HERE
http://saynotodogmeat.net/2014/01/31/turkana-africa-emergency-aid-letter/
EMAIL THE GOVERNOR OF NIGERIA: New Address: info@nigeria.gov.ng
http://saynotodogmeat.net/2013/12/03/email-excellency-dr-honorable-alausa-excellency-honorable-babatunde-fashola/
JOIN THE WORLDWIDE GLOBAL EVENT HERE TODAY
PLEASE EMAIL US A.S.A.P FOR INFORMATION ON HOW YOU CAN HELP. SATURDAY 4TH APRIL 2015 – TIME TO MARCH FOR DOGS AND CATS IN THE MEAT TRADE.
JOIN HERE https://www.facebook.com/events/294347744053559/ SHARE EVERYWHERE WILDLY
Ebola - Global Threat? From the Third World to the Whole World
EBOLA has claimed the lives of some 645 people to-date which is an estimated number, there are still some 1,400 suspected cases (and rising) local to Liberia, Ghana, Sierra Leon and Guinea. One passenger that traveled from Liberia to Nigeria this Friday sadly died from the worlds most dangerous virus, two world health doctors and one nurse have also fallen ill with the highly infectious disease. Unfortunately the nurse that had been treating and helping victims has since died, mocked by her countries minister for having unsafe sex.
Today the British Government announced that one man in Birmingham that is suspected to have traveled from Liberia showed signs of Ebola Hemorrhagic Fever fortunately has since proved negative for mans deadliest virus. Great Britain will today issue its Cobra Meeting of which ministers, military commanders and doctors will be present to discuss and put into plan operations to help combat an Ebola outbreak. Although such a virus outbreak in Europe would be significantly small compared to West Africa the fact British Governmental Ministers have issued the Cobra Meeting of top brass clearly indicates to us that they have something to worry about.
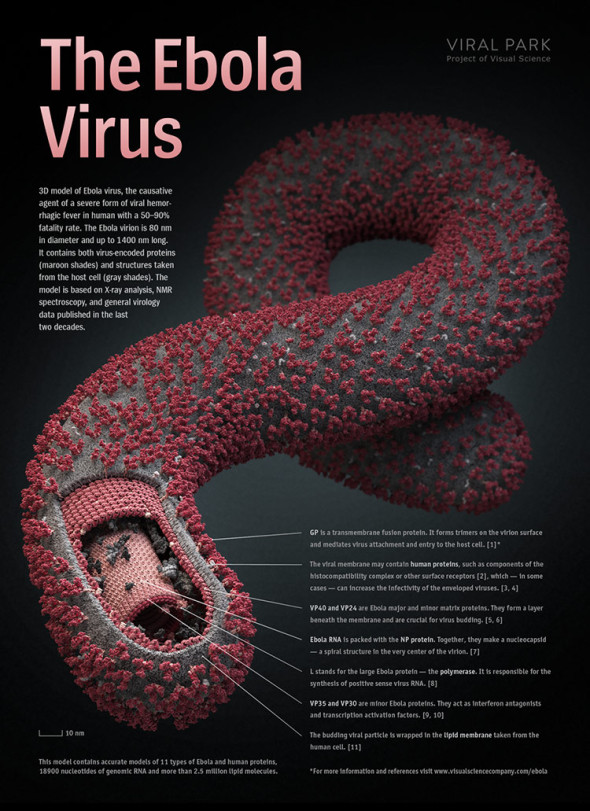
What is Ebola?
Virus, Ebola: A notoriously deadly virus that causes fearsome symptoms, the most prominent being high fever and massive internal bleeding. Ebola virus kills as many as 90% of the people it infects. It is one of the viruses that is capable of causing hemorrhagic (bloody) fever.
Epidemics of Ebola virus have occurred mainly in African countries including Zaire (now the Democratic Republic of Congo), Gabon, Uganda, the Ivory Coast, and Sudan. Ebola virus is a hazard to laboratory workers and, for that matter, anyone who is exposed to it.
Infection with Ebola virus in humans is incidental — humans do not “carry” the virus. The way in which the virus first appears in a human at the start of an outbreak has not been determined. However, it has been hypothesized that the first patient (the index case) becomes infected through contact with an infected animal.
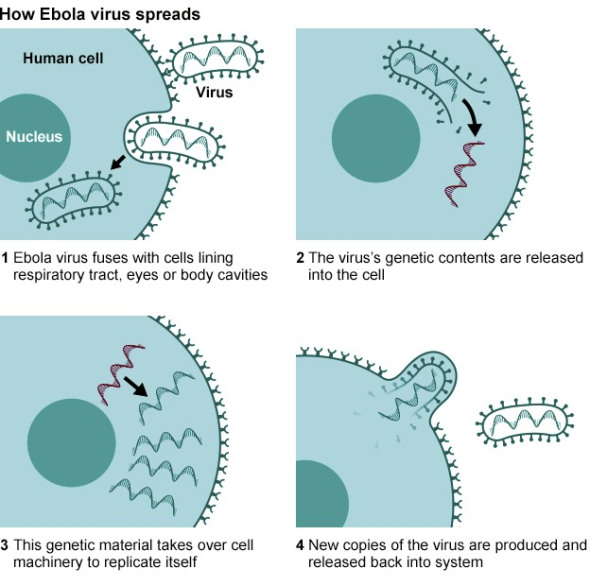
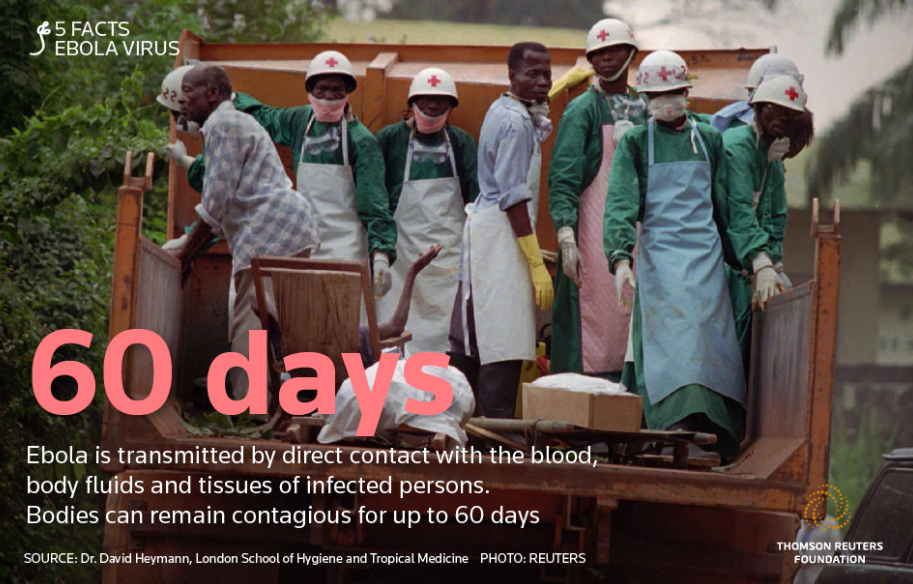
Ebola virus is transmitted by contact with blood, feces or body fluids from an infected person or by direct contact with the virus, as in a laboratory. People can be exposed to Ebola virus from direct contact with the blood or secretions of an infected person. This is why the virus has often been spread through the families and friends of infected persons: in the course of feeding, holding, or otherwise caring for them, family members and friends would come into close contact with such secretions. People can also be exposed to Ebola virus through contact with objects, such as needles, that have been contaminated with infected secretions.
The incubation period -the period between contact with the virus and the appearance of symptoms — ranges from 2 to 21 days.
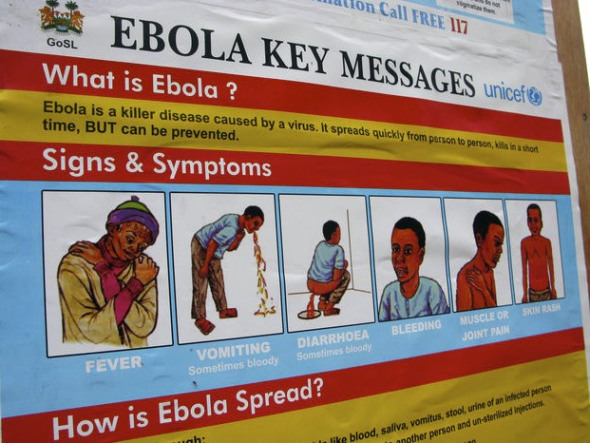
The initial symptoms are usually high fever, headache, muscle aches, stomach pain, and diarrhea. There may also be sore throat, hiccups, and red and itchy eyes. The symptoms that tend to follow include vomiting and rash and bleeding problems with bloody nose (epistaxis), spitting up blood from the lungs (hemoptysis) and vomiting it up from the stomach (hematemesis), and bloody eyes (conjunctival hemorrhages). Then finally come chest pain, shock, and death.
A protein on the surface of the virus has been discovered that is responsible for the severe internal bleeding (the death-dealing feature of the disease). The protein attacks and destroys the endothelial cells lining blood vessels, causing the vessels to leak and bleed.
There is no specific treatment for the disease. Currently, patients receive supportive therapy. This consists of balancing the patient’s fluids and electrolytes, maintaining their oxygen level and blood pressure, and treating them for any complicating infections. Death can occur within 10 days of the onset of symptoms.
The prevention of the spread of Ebola fever involves practical viral hemorrhagic fever isolation precautions, or barrier nursing techniques. These techniques include the wearing of protective clothing, such as masks, gloves, gowns, and goggles; the use of infection-control measures, including complete equipment sterilization; and the isolation of Ebola fever patients from contact with unprotected persons. The aim of all of these techniques is to avoid any person’s contact with the blood or secretions of any patient. If a patient with Ebola fever dies, it is equally important that direct contact with the body of the deceased patient be prevented.
Bioterrorism — There has been concern about Ebola virus as a possible weapon for bioterrorism. However, the General Accounting Office, the investigative arm of the US Congress, in a 1999 report considered Ebola virus to be an “unlikely” biologic threat for terrorism, because the virus is very difficult to obtain and process, unsafe to handle, and relatively unstable.
International Animal Rescue Foundation Africa and their counterparts in Europe, France have been documenting on Ebola since the first outbreak in West Africa 2014 that is now known as the deadliest outbreak thus far. Hon Philip Hammond UK Foreign Secretary will later today BST time hosting the Cobra Committee that will discuss Ebola and what procedures need to be implemented should such a case of Ebola emerge within Great Britain. Few days ago a male in his mid forties began showing signs of Ebola infection however tests thankfully have proved negative. So we know the threat is real and the threat is there. (Click the link to view our Facebook site or contact us via our main communications site)
Dr Josa Depre stated at the start of 2014 when exposing the full scale of pet meat trade within West and North Africa that should Ebola or any virus emerge from the consumption of pet and bush meat the possibilities of “any” such virus emerging into a “super virus” is extremely high, problem is when will it happen. Depre continued that we do not have time to wait for “when it will happen” we must stop trade of bush and pet meat now before such a virus emerges wiping out a quarter of the worlds population.
BAD news is always interesting, especially when it starts small and threatens to grow large, like the little cloud on the distant horizon, no bigger than “a man’s hand,” that is destined to rise as a thunderhead (1 Kings 18:44). That’s why we read so avidly about the recent outbreaks of Ebola virus disease among villages in Uganda and the Democratic Republic of Congo, and about West Nile fever in the area around Dallas (where 15 have died of it since July). And that’s why, early this month, heads turned toward Yosemite National Park after the announcement of a third death from hantavirus pulmonary syndrome among recent visitors there.
Humans die in large numbers every day, every hour, from heart failure and automobile crashes and the dreary effects of poverty; but strange new infectious diseases, even when the death tolls are low, call up a more urgent sort of attention. Why?
There’s a tangle of reasons, no doubt, but one is obvious: whenever an outbreak occurs, we all ask ourselves whether it might herald the Next Big One.
What I mean by the Next Big One is a pandemic of some newly emerging or re-emerging infectious disease, a global health catastrophe in which millions die. The influenza epidemic of 1918-19 was a big one, killing about 50 million people worldwide. The Hong Kong flu of 1968-69 was biggish, causing at least a million deaths. AIDS has killed some 30 million and counting. Scientists who study this subject — virologists, molecular geneticists, epidemiologists, disease ecologists — stress its complexity but tend to agree on a few points.
Yes, there probably will be a Next Big One, they say. It will most likely be caused by a virus, not by a bacterium or some other kind of bug. More specifically, we should expect an RNA virus (specifically, one that bears its genome as a single molecular strand), as distinct from a DNA virus (carrying its info on the reliable double helix, less prone to mutation, therefore less variable and adaptable). Finally, this RNA virus will almost certainly be zoonotic — a pathogen that emerges from some nonhuman animal to infect, and spread among, human beings.
The influenzas are zoonoses. They emerge from wild aquatic birds, sometimes with a pig as an intermediary host on the way to humanity. AIDS is a zoonosis; the pandemic strain of H.I.V. emerged about a century ago from a single Cameroonian chimpanzee. Ebola is a zoonosis. The Ebola viruses (there are five known species) abide inconspicuously in some as yet unidentified creature or creatures native to Central African forests, spilling over occasionally to kill gorillas and chimps and people. SARS is a zoonosis that emerged from a Chinese bat, fanned out of Hong Kong to the wider world, threatened to be the Next Big One, and then was stopped — barely — by fast and excellent medical science.
And the hantaviruses, of which there are many known species (Andes virus, Black Creek Canal virus, Muleshoe virus, Seoul virus, Puumala virus and dozens more), come out of rodents. The species of hantavirus at large in Yosemite is called Sin Nombre — “nameless” — virus, and is the same one that erupted famously, and lethally, at the Four Corners in 1993. Its primary host is the deer mouse, one of the most widely distributed and abundant vertebrates in North America. The virus makes its way from dried mouse urine or feces into airborne dust, and from airborne dust into human lungs. If that happens to you, you’re in trouble. There’s no treatment, and the fatality rate for hantavirus pulmonary syndrome, the infection in severe form, runs at about 40 percent.
You don’t have to go to Yosemite and sleep in a dusty cabin to put yourself close to a hantavirus. Although one expert, recently quoted by Scientific American, called it a “very rare” kind of virus, that view doesn’t square with the studies I’ve read or the testimony of hantavirus researchers I’ve interviewed. The virus seems to be relatively common, at least among deer mice. A 2008 study done at Tuolumne Meadows in Yosemite found that 24 percent of local deer mice had the antibody for the virus, signaling a past or current infection. One mouse in four is worryingly high. Among these mouse populations nationwide, the prevalence of the antibody seems to vary from as low as zero to as high as 49 percent, or one in two mice.
The question this raises is: Why aren’t more people dying from Sin Nombre virus? The answer seems to be that, although very dangerous when caught, it’s not easy to catch, despite its presence in mouse-infested sheds and trailers and garages and barns across much of America. This is because it doesn’t pass from person to person — only from mouse to mouse, and from mouse excretions to one unlucky person or another, each of whom represents a dead-end host. (The “dead” of that “dead-end” may be figurative or literal.) It’s not a “very rare” virus; it’s a common virus known only rarely to infect humans, and with no ramifying chains of human contagion. So the Next Big One is not likely to be Sin Nombre.
Nor is it likely to be Ebola, which is transmissible from human to human through direct contact with bodily fluids, but can be stopped by preventing such contact. Furthermore, Ebola burns so hotly in its victims, incapacitating and killing so quickly, that it is poorly adapted to achieve global dispersal. Only one human has ever been known to leave Africa with a rampant Ebola virus infection — and that was a Swiss woman, evacuated in 1994 to a hospital in Basel. If you want to be grateful for something today, be grateful for that: Ebola doesn’t fly.
WE should recognize such blessings, and try to focus our deepest concerns on real global dangers. Too often, we’re distracted from good scientific information by yellow journalism and the frisson of melodrama. Ebola is charismatic, the demon that people love to fear. Other lurid candidates, like hantavirus and SARS, also get their share of headlines. When you mention emerging diseases, people’s responses tend to fall at the two ends of a spectrum. Some folks are mesmerized by the dark possibilities and the garish but unrepresentative cases. Others are dismissive, rolling their eyes at the prospect of having to contemplate still another category of dire monition. They want you to cut to the chase. “Are we all gonna die?” they ask. Or they say: “Fine, so what can we do about these bugs?”
Yes, we are all going to die, though most of us not from a strange disease newly emerged from a mouse or a chimp. And there are things we can do: get a flu vaccination; support calls for research; avoid coughing people on airplanes; apply mosquito repellent; wear a mask when you sweep out your old shed; don’t eat any chimpanzee meat from an animal found dead in the forest. But the concrete measures are limited by time, place and circumstance. The broader response is more basic: learn, absorb, understand. Don’t start trying to apply your knowledge until you have some.
Among the other unsettling disease news this summer, you’ve probably seen mention of influenza, that old familiar zoonosis, quite capable of devastation and melodrama all its own. Yes, there’s a new flu bug, a nasty variant of the H1N2 strain, suspected now to be traveling through pigs at state fairs. The influenzas are protean and explosive. Keep your eyes on that one.
Hantavirus in Yosemite is a little cloud that seems likely to stay little. This doesn’t mean that the great dark thunderhead isn’t coming. It just speaks to the need for a bit of informed judgment about which sector of the horizon we should watch..
Should a super virus mutation emerge from such species of animals then mass loss of life will be lost. Spanish influenza killed thousands and thousands of people. If such a virus can kill in this manner so can new mutations of Ebola.
Whilst International Animal Rescue Foundation Africa is lobbying for new laws to be implemented to ban pet meat trade within West, North and Central Africa it must be noted that pet meat hosts only a small danger to the public simply because bush meat is considered more a staple diet rather than pet meat which is usually eaten by men rather than women.
Ebola may be present in more animals than previously thought, according to researchers studying the deadly virus, which has already been detected in chimpanzees, gorillas, fruit bats, monkeys, antelopes, porcupines, rodents, dogs, pigs and humans. The close evolutionary relationship between humans, chimpanzees and gorillas makes their immune systems very similar which is of some concern to us.
In general, Ebola researchers think that the natural host of Ebola virus are fruit bats, and that the virus is transmitted to non-human primates and then to humans through the bush meat trade. It is possible that there is direct transmission from fruit bats to humans.
Certain cultures in Africa do consume bat meat, such that Guinea earlier this year ordered a ban on consumption of these flying mammals in an effort to halt the epidemic’s spread. As for how non-human primates might become infected, they often feast on fruits that the bats eat. They can also kill and eat bats, or scavenge meat from infected carcasses.
Then the question remains: How did bats get the virus?
During the deadly Ebola outbreak in Gabon 2001-2002 scientists observed very worrying signs of Ebola virus in dogs too. International Animal Rescue Foundation Africa has documented heavily on the major pet meat consuming countries being that of Liberia, Sierra Leon, Guinea and Ghana. Coincidentally these four African countries are all now experiencing large outbreaks of the Ebola virus. However as explained we must not just blame the pet meat trade here. There are many factors that is not only increasing the virus but spreading too. Poor hygiene, sanitation, denial the virus even exists is common among many West Africans, trading still of bush meat, poverty and handling of the dead that have sadly died from Ebola Hemorrhagic Fever. These being some of the most common issues that are increasing more cases of Ebola emerging.
Scientists observed that several dogs were highly exposed to Ebola virus by eating infected dead animals. To examine whether these animals became infected with Ebola virus, they sampled 439 dogs and screened them by Ebola virus-specific immunoglobulin (Ig) G assay, antigen detection, and viral polymerase chain reaction amplification. Seven (8.9%) of 79 samples from the 2 main towns, 15 (15.2%) of 99 samples from Mekambo, and 40 (25.2%) of 159 samples from villages in the Ebola virus-epidemic area had detectable Ebola virus-IgG, compared to only 2 (2%) of 102 samples from France. Among dogs from villages with both infected animal carcasses and human cases, seroprevalence was 31.8%. A significant positive direct association existed between seroprevalence and the distances to the Ebola virus-epidemic area. This study suggests that dogs can be infected by Ebola virus and that the putative infection is asymptomatic.
Death from denial - Please view the video below;
Ebola virus antibodies were detected in dogs exposed to the virus during the latest epidemics, which suggests that these animals may well have been infected and can therefore be a new source of transmission to humans. Ebola virus infection in humans provokes a violent haemorrhagic fever. It usually flares up as intense epidemics. These kill 80 % of the people infected. Seven such outbreaks have hit Gabon and the Republic of Congo since 1994, leading to 445 cases resulting in 361 deaths. Ebola virus thus constitutes a grave public health problem in these countries. No medicine or vaccine is currently available, only prevention and rapid control of epidemics by isolation of disease victims can limit its spreading.
Moreover, during the latest epidemics in Gabon and the Republic of Congo, there were many cases where dogs had eaten remains of dead animals infected with the virus, nonetheless without showing visible clinical signs. In order to confirm that these dogs had indeed come into contact with the virus, the scientists looked for the presence of specific Ebola virus antibodies in their blood. The percentage of dogs carrying such antibodies increases linearly and significantly the closer they are found to foci of the outbreaks. From 9 % in the two large cities of Gabon, antibody prevalence goes up to 25 % in the untouched villages of the epidemic area, reaching 32 % in the villages where human cases have been attributed to an infected-animal source. These domestic animals could therefore become infected and excrete virus over a given period, thus becoming a potential source of infection for humans. This could explain certain as yet un-elucidated human infections. It now appears necessary to assess the role of dogs in Ebola fever outbreaks and take this risk into account in epidemic-control measures. These animals could furthermore be used as indicators of the presence of the virus in the regions where, besides the appearance of cases of both animal and human deaths, there is no external sign as to whether or not Ebola virus is present.
What is most concerning here is that while many animal hosts show signs of “Ebola” dogs do not which poses an ever more larger threat to humans that are trading dogs in countries such as Liberia and Nigeria. Picture below is that of a dog meat meat market in Nigeria. As one can clearly see here there are many ways in which if that dog did have Ebola could quite easily pass the virus onto the slaughter-men. Skin is exposed, dog is being mishandled and could quite easily pass on via saliva through a broken skin wound deadly Ebola virus. Even more concerning blood hemorrhaging from the cut to the dogs throat can very easily “if” infected with Ebola virus could be passed onto both men should there be an open skin wound, or if hands that come into contact with blood then touch mouths or noses. No masks or protective clothing is being worn as one would see in a slaughterhouse - splattering of blood directly into the face also poses an incredibly high risk of secondary cross infection. From there the virus then takes over the body in under 2-21 says being the incubation period. During that time and if the dog was infected both men that “for example” had been infected would have come into contact with others. Poor sanitation, hygiene, non-safe sexual intercourse and not washing hands after using the bathroom are all major factors of viral contamination passed onto other humans.
Pictured above is also yet another classic sign of a Nigerian dog meat market. Again poor hygiene is seen and not being practiced, the slaughter man is seen holding the dogs mouth of which the dog could harbor both rabies and Ebola. Should saliva from the dog be passed onto the mans hand then “cross contamination” has occurred. Man then touches his mouth or places his fingers into his mouth thus passing on virus. Furthermore as explained above too should the slaughter-man have exposed cuts or abrasions on his feet then splattering of blood again poses a “high risk” of passing on any virus.
How is Ebola passed onto humans from animals?
The virus is transmitted through direct contact with blood or other body fluids of infected persons or animals, including close contact with deceased Ebola-infected patients.
Ebola a risk to non-African countries?
PLEASE read the information below carefully and please also undertake your own research.
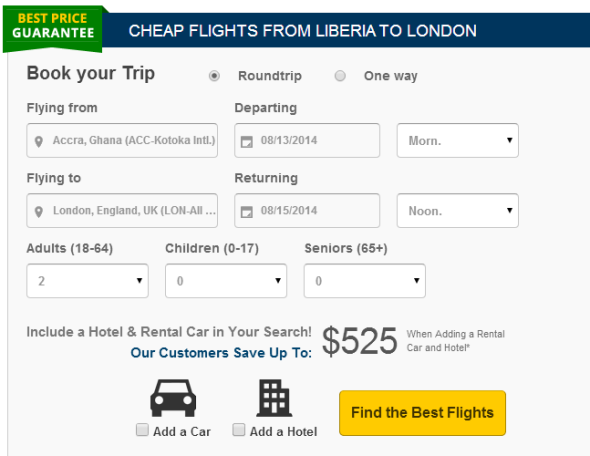
As of today 30th July 2014 the British Government has since launched the Emergency Cobra Committee of which is one of the highest military, health and ministerial meetings within the country. Contingency plans are now being implemented of which all British and now in the last few minutes all European doctors, nurses and border officers are now on full alert with regards to the dangerous risks Ebola poses. While media and the British government have stated there are no direct flights from the “infected zones” directly into the UK there are flights to and from other countries that travel into the UK of which “suspected sufferers” could travel on. Its very irresponsible for the British media and experts to state that just because there are no direct flights from West Africa into Great Britain then risk is minimal. Please view the photo below that depicts a booking our investigative team made from Ghana to London.
The pictures above depicts screenshots that clearly shows how easy it is for anyone within the “infected zones” could very easily travel from West Africa into London. Just because there is no flights directly from (Liberia) doesn’t mean for one single minute that passengers travelling over the border from the Liberia into Ghana can then connect to a direct flight to London from Ghana, Ghana is an infected zone.
In a Facebook response to a question about the country’s preparedness for a possible outbreak, Dr Bampoe said “Yes, Ebola is in the sub-region - the worst outbreak ever, but the Ghana Health Service is well prepared to deal with any case that occurs. There is a misconception that every single health facility in every single district in every single region should have a standing isolation ward, etc. that is neither practical nor feasible”.
He explained “The epidemiology of the disease has changed, and so if we’re going to get a case in Ghana, it will likely be someone traveling from the sub-region. What has been done so far, and what needs to be done?”
“The GHS is working with National Security and the Border agencies to screen people from areas in the sub-region with to spot suspected cases 2. Messages from the Health Service are going out with periodic updates to let people know how to spot suspected cases, who to report them to, how to, avoid getting infected, etc. Much more needs to be done and will be done in this area 3. Each region has been given an allocation of protective equipment that can be rapidly deployed when there is a suspected case. Even before that, health workers are being trained to identify suspected cases and apply barrier nursing” methods, even before the protective equipment are sent,” he disclosed.
Oddly the media has only just reported on this case below 27th July 2014, yet in Ghana the case was reported on the 6th then published in the 7th July 2014.
An American (name withheld) has been quarantined at the Nyaho clinic in Accra for a suspected Ebola case.
City News sources at the Health Ministry say the American who reported at the hospital with fever had previously visited Guinea and Sierra Leone. Hundreds of people have been affected and several others killed by the deadly disease in these two countries.
The Health Ministry in a statement said “the suspected fever case recorded at the Nyaho Clinic has not been confirmed yet by Noguchi Memorial Research Centre”. It further stated that: “the Ministry has put in place every precautionary measure at that clinic, including additional support of Public Health staff from the Ministry, directive to quarantine patient and clinical staff, supply of protective gowns for the staff of that hospital”.
It urged the general public to remain calm as it awaits the results from the blood sample taken for test, insisting that it has the situation under control. Last week, health ministers from all West African countries met in Accra to find ways to stop the disease from spreading. (Since reporting the American has sadly since died) we believe this individual to be a health worker however are very suspicious as to why no name has been issued or other details.
The medical director of Public Health England said it was “unlikely but not impossible” that travellers infected in West Africa could develop symptoms on their return. According to Dr Ben Neuman, a virologist at Reading University, the chance of the virus spreading in the UK was “very, very small”.
He said border staff are already trained to deal with illnesses of this kind, and anyone showing signs of fever from an outbreak area would be stopped, quarantined and treated in containment facilities if the infection were confirmed.
He said the virus itself is “delicate and inefficient - you have to pick it up from bodily fluids”. But he said it was sensible to be prepared, given the situation in West Africa.
While the medical director of Public Health England has stated the risk is “very, very, small” the risk is still there. Anyone travelling from West African directly into the UK or America that are not actually showing any signs of Ebola can infect passengers on the place via fecal transmission within toilet cubicles, vomiting on the plane of which passes bodily fluids onto others. International Animal Rescue Foundation Africa has requested the British Border Agency and airway companies that are ferrying passengers from West Africa into Europe to now implement a temporary ban with immediate affect. As explained while there is a small risk the risk is still there and we cannot take any risks or slip up.
Since 1976 there has been no confirmed cases of Ebola Hemorrhagic Fever ever confirmed within Great Britain. Today’s case was fortunately negative but how many cases has there been recorded since the worlds deadliest virus emerged? See information below.
Ebola Hemorrhagic Fever deaths to date are reported below. Why has the number of cases jumped sporadically since 1976 to 2014?
- Zaire 1976 = 280 deaths
- Sudan 1976 = 151 deaths
- Zaire 1977 = 1 death
- Sudan 1979 = 22 deaths
- USA 1990 = 4 cases = no deaths
- Philippines 1990 = 3 cases = no deaths
- Gabon 1994 = 31 deaths
- Ivory Coast = 1 case = no deaths
- Democratic Republic of Congo 1995 = 250 deaths
- Gabon 1996 = 21 deaths
- Gabon 1997 = 45 deaths
- South Africa 1996 - 97 = 1 death
- Uganda 2001 = 224 deaths
- Gabon 2002 = 53 deaths
- Republic of Congo 2002 = 43 deaths
- Republic of Congo 2003 = 128 deaths
- Republic of Congo (Nov-Dec) = 29 deaths
- Sudan 2004 = 7 deaths
- Democratic Republic of Congo 2007 = 187 deaths
- Uganda 2008 = 37 deaths
- Philippines 2008 = 6 cases = no deaths
- Democratic of Congo 2009 = 14 deaths
- Uganda 2012 = 17 deaths
- Democratic Republic of Congo 2012 = 36 deaths
- Guinea, Liberia, Sierra Leone, Nigeria = estimated total under 670 deaths and rising
- Great Britain 2014 = 1 suspected case = negative - no deaths
There has been some speculation as to why the number of cases of Ebola virus has increased from 1970 to 2014;
- Human over population is increasing which in turn reduces land mass that can be used for sustainable agriculture.
- Climate change has affected many African countries of which see’s crop reduction and cattle death due to lack of rain fall and suitable climatic conditions suitable to sustain a healthy non-bush meat diet.
- Wildlife has taken a drastic decline within West Africa - one prime example of this is Liberia where many species of old and new primates, mammals and birds are declining. Whilst these species of animals are used in the trade of bush meat with very few species remaining pet meat is the only readily solution to halt starvation and malnutrition.
- Civil war in Sierra Leone and Liberia has left the two countries tarnished with many people living in poverty and illiterate. Starvation is common and while many people remain impoverished the only suitable meats to them are cheap pet meat or dead carrion laying on the forest floor. Many people within West Africa are illiterate so simple education and awareness of such unhealthy eating and the dangers surrounding pet and bush meat trade is easier said than understood.
- Witchcraft and traditional black medicine is cheap and seen as more healthier alternative to synthetic medications. While many people in West Africa believe such traditions actually decrease highly infectious diseases and virus fact is there is no clinical evidence whatsoever to prove such traditions actually benefit humans.
- Denial and lack of education has played quite a pivotal role in allowing Ebola in this case to increase killing over 650 victims. Many West African citizens do not believe Ebola actually exists and that their government are trying to scare monger international agencies into sending more funding to them of which is a myth. With lack of funding there comes lack of education - International Animal Rescue Foundation Africa are now helping to fund school classes in West Africa on the dangers of Ebola, SARS, H1N1 and rabies.
- Lack of employment has driven many West Africans to trade in pet and bush meat regardless of the dangers it poses. Liberia and Ghana has banned the bush meat and pet meat trade however locals cannot survive without an income so therefore trade has continued.
- Increased handling of infected chimpanzees, gorillas, fruit bats, monkeys, forest antelope and porcupines found ill or dead or in the rainforest.
Josa Depre when questioned yesterday stated the following;
AS WE live in an interconnected world–and not just by the internet- we have to come to grips with the fact that hopping on a plane may potentially spread any virus–not just Ebola–to another country. Thus, the importance of enforcing proper infectious screening procedures of those who plan to board an aircraft in an endemic area such as West Africa becomes critical to containing the spread of the Ebola virus. Enforcing a “Do Not Board List” would be critical to preventing any spread of such a virus. Still noo such (DNB) has been issued and for all we know an Ebola carrier could be living next door to us, sitting on the same plane as anyone of us, on the same train as us that has left the infected zone to visit relatives or conduct business.
AND NO this is not a black persons illness. Just because the virus is rife in West Africa doesn’t mean for one minute that white people cannot become infected too. This is a myth that carries with it much racial hatred too. Josa Depre stated “Anyone can catch Ebola, you do not have to consume dog, cat or even eat bush meat, you could accidentally come into contact with an infected persons bodily fluid by any-means”. “That infected person may also not have consumed the later but actually be present at the death of a loved one, tending their bodies, or have accidentally come into contact with a dog from licking of ones face, dogs are known to scavenge on the forest floor for carrion, then travelling back into the community is a death sentence in itself”. “This is the problem we are facing in West Africa and until those over the borders in other countries start pulling their weight and helping in anyway possible were going to see more mass deaths, more infected people, more mass panic we could even see people migrating from the infected zones into Southern Africa where tourists flock in their thousands”, “It may already be happening, we cannot control people from moving out, borders are unmanned, What do we do, we need help” stated the Chief Executive Officer.
WHILE the Ebola virus could potentially be transported by travelers to another country by a plane ride, according to officials at the CDC, the actual chance of this developing into a serious public health risk to those living in the US is small. The reason for this is due to good professional health practices and experience in containing highly contagious infectious diseases. Josa stated though “Public and governments could be caught unaware” “For instance if person A carrying the virus from (day 2-21) traveled to America from Liberia infected person B travelling to Minnesota then person B will then carry while in the incubation period (showing little or no signs of infection) Ebola virus to person C,D,E and F” “While still in the incubation period what if persons C,D,E and more that had contracted the virus then go on to travel further or infect those in the work place” “Could health organisations quickly trace and confine such a disease?” The answer to that question can only be answered when and if the virus hits (which we hope doesn’t).
ONE of the main reasons, officials believe, that the virus has a low public health risk is related to the conditions which would be favorable to allow spread of the virus. Poor and crowded living conditions, along with improper sanitation seem to be an important element that contribute to the spread of the virus. Such are not the living conditions, in general, throughout most modernized countries in the Western world. Health officials seem to be forgetting something though, the poor, elderly, those living in slums, schools and high crowded public areas. “It takes just one person to infect 2 then 4 then 8 then we have major problems, THE manner in which this virus spreads is no different to that of highly contagious virus’s that are spread by direct or indirect contact stated Josa Depre”. Public areas such as schools, bars, work places and more are “high risk”. Good sanitation means nothing when the virus IF the virus has entered then been passed on - We must be vigilant and ready stated Depre.
For now the only “real” threat as stated by health officials is that of infected persons travelling on flights to and from Africa. However as explained infected people within the first stages of incubation show signs not even typical of Ebola virus. Minor fever, restlessness, some nausea and diarrhea, headache and tiredness can easily be mistaken as a mere common cold. While travel agencies and flight crew have to keep to strict time schedules and still undertake their daily routine jobs its very easy for anyone to pass by border or cabin crew thus then placing others in danger. We’ve already seen two such cases this month although one in Nigeria was positive in the United Kingdom, Birmingham this proved negative. It clearly shows though how easily these two individuals have passed by on planes, gone unchecked by border and airway crew even though Ebola virus has been ravaging West Africa for the past three months. How many more cases are there out there that we do not know of?
International Animal Rescue Foundation Africa believes now that West Africa must impose a complete travel ban on all citizens within the infected zones and all international countries to now ban those from travelling via West Africa into international waters regardless to whether the risks are very, very small. As soon as we let our guard down we become the victims.
There is no cure for Ebola virus disease, no established drug therapy to treat Ebola infection, and no vaccine that can protect humans against Ebola. Scientists lack sufficient diagnostic tools to rapidly identify Ebola infections. Scientists also need a more thorough understanding about how the virus is transmitted and how it causes disease. Ebola is a threat not only to humans but also to our closest living relatives - the great apes. The western lowland gorilla populations have been decimated by Ebola to such an extent that they are now considered “critically endangered”. About a third of the gorillas in protected areas have died from Ebola in the past 15 years. Scientists are concerned that their numbers may not be able to recover and fear that they could become extinct in as soon as a decade.
In addition to being classified as a potential bioterrorism agent, the risk of continued natural outbreaks or the further emergence of Ebola is a serious concern. As the human population grows, human contact with bats or Ebola-infected non-human primates increases. The discovery of the Reston subtype of Ebola virus in pigs introduces the additional possibility of transfer of Ebola virus to humans from pigs. Although the Reston subtype has not caused illness in humans to date, it is possible that the virus could become more dangerous after passage through pigs because they are ideal hosts in which viruses can mix and mutate.
Thank you for reading;
Chief Executive Officer Europe
DONATE HERE or via our communications site HERE
Thank you. Your donation large or small is used to help dogs and cats in the meat trade, rabies awareness and education, reduce dog bites, vaccination spay and neuter. Furthermore any donation is much appreciated that also travels directly to our FAWS project to help reduce anti-poaching, purchase much needed Anti Poaching equipment and to help the many orphaned wild animals caught up in horrifying wildlife trade. For more information please contact us below.
Contact us HERE
Dog Meat Trade & Ebola.
International Animal Rescue Foundation Africa has been researching in depth the dog and cat meat trade all over Africa since 2012.
Worryingly news is now emerging that the Ebola virus a killer has been noted within the African states listed herein of which there is an active bushmeat trade and pet trade. Furthermore there is also decreased levels of wildlife within these areas compared to that of Southern Africa and East Africa.
Please view the research below that is related to dogs and Ebola. Research was conducted by Centers for Disease Control and Prevention
During the 2001–2002 outbreak in Gabon, we observed that several dogs were highly exposed to Ebola virus by eating infected dead animals. To examine whether these animals became infected with Ebola virus, we sampled 439 dogs and screened them by Ebola virus–specific immunoglobulin (Ig) G assay, antigen detection, and viral polymerase chain reaction amplification. Seven (8.9%) of 79 samples from the 2 main towns, 15 (15.2%) of 14 the 99 samples from Mekambo, and 40 (25.2%) of 159 samples from villages in the Ebola virus–epidemic area had detectable Ebola virus–IgG, compared to only 2 (2%) of 102 samples from France. Among dogs from villages with both infected animal carcasses and human cases, seroprevalence was 31.8%. A significant positive direct association existed between seroprevalence and the distances to the Ebola virus–epidemic area. This study suggests that dogs can be infected by Ebola virus and that the putative infection is asymptomatic.
Picture (1) depicts areas where Ebola has been documented and states of Africa that have a known dog and bush meat trade. Areas too where dog and cat meat is consumed of which have yet to see any documented evidence of Ebola as yet. As you can see all the above African states are widely known to consume dog meat of which Nigeria is the largest trafficker and consumer nation. Is it not much of a coincidence that these are the only areas where dogs and cats are consumed of which Ebola has broken out. Nigeria, Mali, Ghana and Senegal have yet to document on any such cases. If this is not a coincidence then we leave you with the question, where has Ebola really derived from? No known cases have been reported in East Africa or Southern Africa to date.
During the past 3 years, 5 Ebola outbreaks due to Ebola virus-Z have struck the region of central Africa, including Gabon and Republic of Congo, and caused 334 deaths among the 428 reported human cases. In previous studies, it was showed that each extended outbreak could be subdivided into several independent epidemic clusters or chains of transmission, which resulted from close contact with an Ebola virus-Z–infected animal carcass. Epidemiologic observations and genetic analyses identified gorilla, chimpanzee, and duiker carcasses as the main sources of human cases. It must be noted too that stray dogs will consume dead wildlife meat that could be infected with Ebola. Once the species barrier has been crossed between animals and humans, the disease spreads among humans by direct physical contact.
Some human cases in the recent outbreak in the Gabon/Republic of Congo region did not have a documented source of exposure to Ebola hemorrhagic fever. Similarly, 14 (4.9%) of the 284 cases in the 1976 Sudan outbreak (6) and 55 (17.4%) of the 316 cases during the 1995 outbreak in Kikwit (7), Democratic Republic of Congo (DRC, former Zaire), had no direct physical contact with an infected person or known infected carcass. These observations point to other routes of transmission (e.g., human-human respiratory tract infection through droplets and aerosols) or may suggest that other, unidentified animal sources may be involved in Ebola virus transmission to humans.
Ebola hemorrhagic fever outbreaks occurred in villages where people keep domestic animals, including dogs. The dogs are not fed and have to scavenge for their food. They eat small dead animals found near the villages and also internal organs of wild animals hunted and slaughtered by villagers. Some dogs are also used for hunting in the dense forested area. Although canine infection by Ebola virus has never been documented, domestic dogs’ behavior and diet place them at risk.
Scientists examined whether pet dogs could have been infected by Ebola virus and their potential role as primary or secondary sources of human infection. Researchers conducted a large-scale serologic survey to determine the prevalence of Ebola virus infection in pet dogs in an Ebola virus–epidemic area of Gabon.
Sampling was conducted in 2 ways. 1) Dogs in Libreville and Port Gentil were sampled in a veterinary clinic. Blood was collected in 5-mL dry Vacutainers (VWR International, Fontenay-sous-bois, France), and serum was prepared by centrifugation. Serum specimens were stored at –20°C until they were sent to the Centre International de Recherches Médicales de Franceville (CIRMF), Gabon, where they were stored at –80°C until testing. 2) Dogs from the Ebola virus–endemic area were sampled in the villages. An experienced veterinary team was located at Mekambo, where field laboratory facilities were set up; blood samples were collected on a daily basis in the vicinity of the village by using 5-mL dry Vacutainers and medetomidine anesthesia. The tubes were then transported to Mekambo each evening, and serum was decanted from whole blood. Serum samples were kept in liquid nitrogen in 1-mL aliquots at Mekambo until they were transported to CIRMF. Serum samples were then stored at –80°C until serologic testing, antigen detection, and RNA amplification were carried out.
Dog owners were interviewed on their pets’ activities (e.g., participation in hunting) and health history. The focus of the interviews was on potential Ebola virus–exposure events, including human cases that occurred in the village and among dog owners.
Laboratory Investigations
Ebola virus–specific immunoglobulin (Ig) G was detected by using a standard enzyme-linked immunosorbent assay (ELISA) method as previously described (8). Briefly, Maxisorp plates (VWR International) were coated with Ebola virus–Z antigens diluted 1:1,000 in phosphate-buffered saline (PBS), overnight at 4°C. Control plates were coated with uninfected Vero cell culture antigens in the same conditions. Sera diluted 1:400 in 5% nonfat milk in PBS-Tween 20 (0.1%) were added to the wells and incubated overnight at 4°C. IgG binding was visualized by using a peroxidase-labeled anti-dog IgG (Kirkegaard & Perry Laboratories, Inc., Gaithersburg, MD, USA) and the TMB detector system (Dynex Technologies, Issy-les-Moulineaux, France). Optical density (OD) was measured at 450 nm with an ELISA plate reader. For each sample we calculated the corrected OD as the OD of the antigen-coated well minus the OD of the corresponding control well. The cut-off value (CO) was calculated as follows: CO = M + 3σ, where M is the average of the corrected OD of the 102 negative controls from France, and σ is the standard deviation. Samples were considered positive when the corrected OD was above the cut-off.
Samples positive in these serologic assays were used for antigen detection (9) and for viral polymerase chain reaction (PCR) amplification (10). Three positive and 3 negative serum specimens were also used for virus isolation (9). Briefly, Maxisorp plates were coated with a cocktail of 7 monoclonal antibodies against Ebola virus–Z antigens; control plates were coated with normal mouse ascitic fluid produced from the parent myeloma cell line. Serum was then added to the wells, followed by hyperimmune rabbit Ebola polyvalent antiserum and then peroxidase-conjugated goat antibodies against rabbit IgG. The TMB Microwell peroxidase substrate system was used to measure OD. For the detection of viral mRNA, total RNA was isolated from serum with the QIAmp viral RNA kit (Qiagen, Courtaboeuf, France), and cDNA was synthesized from mRNA as previously described. Two pairs of degenerate primers corresponding to the L-gene of Ebola virus were used for 2 rounds of amplification, which yielded a 298-bp fragment.
Statistical Methods
Confidence intervals for proportions were calculated by using the Clopper and Pearson method (11). Statistical comparisons between seroprevalence rates according to the sampling area were performed by using the Fisher exact test. The Cochran-Armitage test was used as a trend test for proportions, after checking for the goodness-of-fit of the underlying linear model (12). All tests used a 0.05 significance level. Statistical analyses were performed by using R software (R Development Core Team; 13).
Results
A total of 439 blood samples from dogs were screened for Ebola virus–specific IgG. Two (2%) of the 102 blood samples from dogs living in France had detectable Ebola virus–reactive IgG (Table 2). Seven of the 79 dogs sampled in Libreville and Port Gentil (8.9% prevalence rate), 15 of the 99 dogs sampled in Mekambo (15.2% prevalence rate), and 40 of the 159 dogs sampled in villages located within the Ebola virus–epidemic area (25.2% prevalence rate) had detectable IgG to Ebola virus antigens.
During the 2001–2002 Ebola outbreak in Gabon, human cases of Ebola virus infection appeared only in certain villages within the Ebola virus–epidemic area (Figure 1). The prevalence of Ebola virus-reactive IgG among dogs from the villages where humans cases occurred was 27.2%, compared to 22.4% among dogs from villages where no human cases were noted (Table 2). In some cases, hunters had brought back to the village an Ebola virus–infected animal carcass found in the forest. This carcass was the source of human infection in the village, and the disease then spread from human to human, both within the village and to other villages by population movement. Thus, only secondary human cases were observed in some villages, with no identified animal source. The prevalence rate among dogs from villages with both an animal source and human cases was as high as 31.8%, compared to 15.4% among dogs from villages with human cases but no identified animal source.
In conclusion, this study offers the first evidence that dogs might be asymptomatically infected by Ebola virus in the wild. This finding has potential implications for preventing and controlling human outbreaks. The increasing canine seroprevalence gradient from low-risk to at-risk Ebola virus–endemic areas indicates that this seroprevalence might be used as an epidemiologic indicator of virus circulation in regions where no other means of virus detection are available.
Read the entire study here now;
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3298261/
WHO quotes nothing about the transmission of Ebola from dogs to humans which is worrying.
Ebola is introduced into the human population through close contact with the blood, secretions, organs or other bodily fluids of infected animals. In Africa, infection has been documented through the handling of infected chimpanzees, gorillas, fruit bats, monkeys, forest antelope and porcupines found ill or dead or in the rainforest.
Ebola then spreads in the community through human-to-human transmission, with infection resulting from direct contact (through broken skin or mucous membranes) with the blood, secretions, organs or other bodily fluids of infected people, and indirect contact with environments contaminated with such fluids. Burial ceremonies in which mourners have direct contact with the body of the deceased person can also play a role in the transmission of Ebola. Men who have recovered from the disease can still transmit the virus through their semen for up to 7 weeks after recovery from illness.
Health-care workers have frequently been infected while treating patients with suspected or confirmed EVD. This has occurred through close contact with patients when infection control precautions are not strictly practiced.
Among workers in contact with monkeys or pigs infected with Reston ebolavirus, several infections have been documented in people who were clinically asymptomatic. Thus, RESTV appears less capable of causing disease in humans than other Ebola species.
However, the only available evidence available comes from healthy adult males. It would be premature to extrapolate the health effects of the virus to all population groups, such as immuno-compromised persons, persons with underlying medical conditions, pregnant women and children. More studies of RESTV are needed before definitive conclusions can be drawn about the pathogenicity and virulence of this virus in humans.
Signs and symptoms
EVD is a severe acute viral illness often characterized by the sudden onset of fever, intense weakness, muscle pain, headache and sore throat. This is followed by vomiting, diarrhoea, rash, impaired kidney and liver function, and in some cases, both internal and external bleeding. Laboratory findings include low white blood cell and platelet counts and elevated liver enzymes.
People are infectious as long as their blood and secretions contain the virus. Ebola virus was isolated from semen 61 days after onset of illness in a man who was infected in a laboratory.
The incubation period, that is, the time interval from infection with the virus to onset of symptoms, is 2 to 21 days.
Diagnosis
Other diseases that should be ruled out before a diagnosis of EVD can be made include: malaria, typhoid fever, shigellosis, cholera, leptospirosis, plague, rickettsiosis, relapsing fever, meningitis, hepatitis and other viral haemorrhagic fevers.
Ebola virus infections can be diagnosed definitively in a laboratory through several types of tests:
- enzyme-linked immunosorbent assay (ELISA)
- antigen detection tests
- serum neutralization test
- reverse transcriptase polymerase chain reaction (RT-PCR) assay
- virus isolation by cell culture.
Samples from patients are an extreme biohazard risk; testing should be conducted under maximum biological containment conditions.
Prevention and treatment
No vaccine for EVD is available. Several vaccines are being tested, but none are available for clinical use.
Severely ill patients require intensive supportive care. Patients are frequently dehydrated and require oral rehydration with solutions containing electrolytes or intravenous fluids.
No specific treatment is available. New drug therapies are being evaluated.
Natural host of Ebola virus
In Africa, fruit bats, particularly species of the genera Hypsignathus monstrosus, Epomops franqueti and Myonycteris torquata, are considered possible natural hosts for Ebola virus. As a result, the geographic distribution of Ebolaviruses may overlap with the range of the fruit bats.
Ebola virus in animals
Although non-human primates have been a source of infection for humans, they are not thought to be the reservoir but rather an accidental host like human beings. Since 1994, Ebola outbreaks from the EBOV and TAFV species have been observed in chimpanzees and gorillas.
RESTV has caused severe EVD outbreaks in macaque monkeys (Macaca fascicularis) farmed in Philippines and detected in monkeys imported into the USA in 1989, 1990 and 1996, and in monkeys imported to Italy from Philippines in 1992.
Since 2008, RESTV viruses have been detected during several outbreaks of a deadly disease in pigs in Philippines and China. Asymptomatic infection in pigs has been reported and experimental inoculations have shown that RESTV cannot cause disease in pigs.
Prevention
Controlling Ebola Reston in domestic animals
No animal vaccine against RESTV is available. Routine cleaning and disinfection of pig or monkey farms (with sodium hypochlorite or other detergents) should be effective in inactivating the virus.
If an outbreak is suspected, the premises should be quarantined immediately. Culling of infected animals, with close supervision of burial or incineration of carcasses, may be necessary to reduce the risk of animal-to-human transmission. Restricting or banning the movement of animals from infected farms to other areas can reduce the spread of the disease.
As RESTV outbreaks in pigs and monkeys have preceded human infections, the establishment of an active animal health surveillance system to detect new cases is essential in providing early warning for veterinary and human public health authorities.
Reducing the risk of Ebola infection in people
In the absence of effective treatment and a human vaccine, raising awareness of the risk factors for Ebola infection and the protective measures individuals can take is the only way to reduce human infection and death.
In Africa, during EVD outbreaks, educational public health messages for risk reduction should focus on several factors:
- Reducing the risk of wildlife-to-human transmission from contact with infected fruit bats or monkeys/apes and the consumption of their raw meat. Animals should be handled with gloves and other appropriate protective clothing. Animal products (blood and meat) should be thoroughly cooked before consumption.
- Reducing the risk of human-to-human transmission in the community arising from direct or close contact with infected patients, particularly with their bodily fluids. Close physical contact with Ebola patients should be avoided. Gloves and appropriate personal protective equipment should be worn when taking care of ill patients at home. Regular hand washing is required after visiting patients in hospital, as well as after taking care of patients at home.
- Communities affected by Ebola should inform the population about the nature of the disease and about outbreak containment measures, including burial of the dead. People who have died from Ebola should be promptly and safely buried.
Pig farms in Africa can play a role in the amplification of infection because of the presence of fruit bats on these farms. Appropriate biosecurity measures should be in place to limit transmission. For RESTV, educational public health messages should focus on reducing the risk of pig-to-human transmission as a result of unsafe animal husbandry and slaughtering practices, and unsafe consumption of fresh blood, raw milk or animal tissue. Gloves and other appropriate protective clothing should be worn when handling sick animals or their tissues and when slaughtering animals. In regions where RESTV has been reported in pigs, all animal products (blood, meat and milk) should be thoroughly cooked before eating.
Controlling infection in health-care settings
Human-to-human transmission of the Ebola virus is primarily associated with direct or indirect contact with blood and body fluids. Transmission to health-care workers has been reported when appropriate infection control measures have not been observed.
It is not always possible to identify patients with EBV early because initial symptoms may be non-specific. For this reason, it is important that health-care workers apply standard precautions consistently with all patients – regardless of their diagnosis – in all work practices at all times. These include basic hand hygiene, respiratory hygiene, the use of personal protective equipment (according to the risk of splashes or other contact with infected materials), safe injection practices and safe burial practices.
Health-care workers caring for patients with suspected or confirmed Ebola virus should apply, in addition to standard precautions, other infection control measures to avoid any exposure to the patient’s blood and body fluids and direct unprotected contact with the possibly contaminated environment. When in close contact (within 1 metre) of patients with EBV, health-care workers should wear face protection (a face shield or a medical mask and goggles), a clean, non-sterile long-sleeved gown, and gloves (sterile gloves for some procedures).
Laboratory workers are also at risk. Samples taken from suspected human and animal Ebola cases for diagnosis should be handled by trained staff and processed in suitably equipped laboratories.
View more within the video below.
International Animal Rescue Foundation and Say No To Dog Meat.Net whom are not affiliated with us have been stating now for many months that dog and cat meat trade “will pose a significant health risk” in viral format to the global population unless the trade is ceased. Could the Ebola outbreak now be one of these major global concerns and if so why has not one single government lobbied by us and SNTDM actually taken this on board. We will most likely never know where the Ebola outbreak originated from. This is plausible evidence though that Ebola can be transmitted from dogs to humans and from dogs that have brought back infested Ebola meat to human villages. Is it such a coincidence too that Ebola has only been recorded within Western Africa where dog, cat and bush meat is consumed and where poverty, climate change, civil unrest and lack of wildlife species is common place. Only one single case of Ebola this year as been recorded within Southern Africa that we are aware of.
We have highlighted this issue in the hope that someone within the virial community will investigate in-depth the possible relations of consuming dogs and bush meat and Ebola virus documenting a detailed response to our concerns as to why Ebola has only been recorded within Western Africa. Bush meat is consumed all over Africa, yet dog meat is consumed only by small minorities with the exception of Nigeria. Coincidence or are the authorities concealing what they have actually ignored?
Whatever the answer this must be a wake up call to the entire African continent now before its to late.